Why Should I Bring my Pet to Willows for Hyperadrenocorticism (HCA)?
Willows is one of Europe’s leading small animal referral centres. Our state-of-the-art hospital is led by internationally renowned Specialists, to providing the highest standards of veterinary care. Diagnosing HAC can be a challenge as there is no single test which can be used to confirm the diagnosis. At Willows our team of Internal Medicine Specialists are highly experienced at the interpretation of laboratory results and work closely with the Specialist Diagnostic Imaging team who perform ultrasound or CT scans to help achieve a diagnosis in these patients.
All of which is supported by our dedicated team of Nurses and clinical support staff are available 24 hours a day, every day of the year to provide the best possible care for your pet.
What is Hyperadrenocorticism?
Hyperadrenocorticism (HAC), also known as Cushing’s Disease or Syndrome, is a condition caused by long-term exposure to high concentrations of cortisol, a glucocorticoid steroid hormone which is necessary for life and is normally produced in response to stress by the adrenal glands (two small glands located near the kidneys in the abdomen).
What are the Most Common Causes of Hyperadrenocorticism?
The most common cause (85% of cases) of HAC is a benign tumour in the pituitary gland located at the base of the brain which is called pituitary-dependent hyperadrenocorticism (PDH). In PDH the pituitary gland produces high amounts of a hormone (adrenocorticotrophic hormone or ACTH) which stimulates cortisol production by the adrenal glands. Approximately 15% of dogs with HAC have a tumour in one (rarely both) adrenal glands which produces excess cortisol whilst the other adrenal glands stops functioning, known as adrenal-dependent hyperadrenocorticism (ADH).
What are the Signs of Hyperadrenocorticism?
The most common signs are drinking and urinating excessively, increased appetite, excessive panting, thin skin and sparse hair coat, weakness and muscle wastage and a distended abdomen with a pot-bellied appearance. Dogs with HAC are prone to infections such as urinary tract infection and uncontrolled diabetes (see Diabetes mellitus information sheet).

How is it Diagnosed?
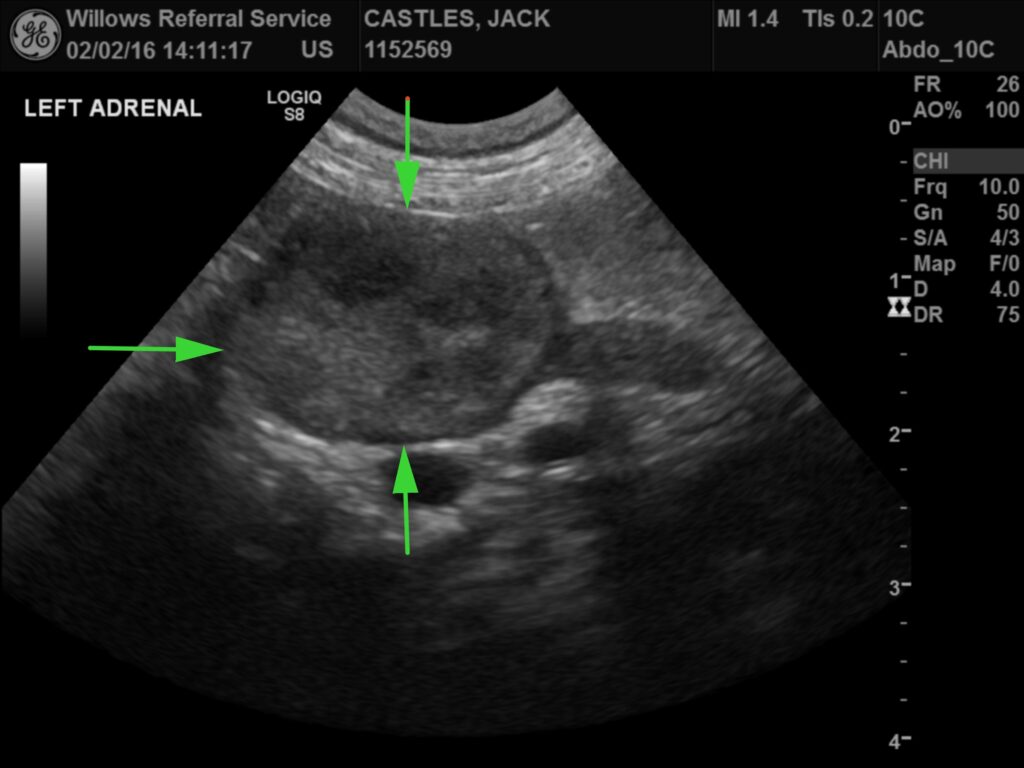
Diagnosis of HAC requires a full history, detailed physical examination, routine blood, urine tests and hormone tests. Diagnostic imaging such as an ultrasound scan of the abdomen (image 1) or a CT scan of the abdomen or brain (image 2) are required to help confirm the diagnosis or differentiate between PDH and ADH. HAC can be very hard to diagnose as the disease can have similar symptoms to other diseases and hormone test results can be falsely positive with some of these other diseases mimicking HAC. Falsely negative hormone results can also occur in some dogs with HAC.
Fig 1: Abdominal ultrasound scan showing an adrenal gland mass

What are the Treatments Available?
The treatment of PDH differs from ADH. Dogs with PDH are treated with medications whereas surgery is usually recommended in dogs with an adrenal gland tumour. The most common medication used in the UK to treat PDH is trilostane (Vetoryl®). This treatment is given once or twice a day as a capsule. Trilostane reduces the production of excessive amounts of cortisol. It can have powerful effects, and it is therefore important that blood tests are performed at intervals to measure the amount of cortisol produced. Too much medication can cause vomiting, diarrhoea, lack of appetite and weakness. Surgery to remove the adrenal gland is usually recommended for ADH although the symptoms of HAC can also be managed with trilostane. This surgery is complicated and is performed by our Specialist team of Anaesthetists and Surgeons. If surgery is an option, this will be discussed with you in detail to ensure that you are fully informed of all the significant implications of the procedure.
Fig 2: CT scan showing a mass in the pituitary gland in the brain
What Can I Expect if my Pet is Treated for Hyperadrenocorticism?
Dogs treated with trilostane usually require this life-long with dose adjustments made dependent on their response. Within a few days of starting treatment the signs of increased thirst, urination and appetite should start to improve. Symptoms such as hair loss and abdominal enlargement take several months to completely resolve. Blood tests are required after one month and approximately every three months, depending upon the response to treatment.
Long Term Management
Although HAC is quite a serious disease which can affect life expectancy, we will do all we can to enable a patient to enjoy a good quality of life, hopefully for a long time to come. In most cases, the earlier the condition is diagnosed and the more closely the effects of treatment are monitored, the better the outlook will be.
To save this page as a PDF, click the button and make sure “Save as PDF” is selected.
Internal Medicine
Find out more
To assist owners in understanding more about Internal Medicine we have put together a range of information sheets to talk you through the some of the more common Medicine conditions seen and treated by our Specialists.

