Why Should I Bring my Dog to Willows for Diagnosis and Management of Lymphoma?
Willows is one the UKs only referral centres to have full-time Specialists in both the Medical and Surgical of tumour diagnosis and management. This, combined with a multi-disciplinary team approach to the management of pets with cancer, enables Willows to provide the best possible levels of care to our patients. Clinical care for cancer patients is provided by Specialists in Oncology, Soft Tissue Surgery and Internal Medicine.
These services are fully supported by Specialists in Diagnostic Imaging, Anaesthesia, Emergency and Critical Care, Clinical Nutrition and by our dedicated Interns, Nurses and Clinical support staff who provide care 24 hours a day, 365 days of the year.
What is Lymphoma?
Lymphoma is a cancer of the lymphatic system. The lymphatic system is, amongst other things, involved in immunity and fighting infections. Lymphoma arises from cells in the lymphatic system called lymphocytes which normally travel around the body, and so this form of cancer is usually widespread. Lymph nodes (sometimes called lymph glands) are part of the lymphatic system and are located all over the body. Lymphoma can affect some or all of the lymph nodes at the same time.
It may be possible to feel or see affected lymph nodes that are near the body surface (as shown in the picture below), they usually feel big and firm. Lymph nodes deeper inside the body are also often involved, as well as internal organs such as the liver, spleen, and bone marrow. This widespread involvement is not like tumour spread in other types of cancer.
What Lymph nodes you can feel?
- Submandibular: under the jaw
- Prescapular: in front of the shoulder
- Axillary: in the armpit
- Inguinal: in the groin
- Popliteal: behind the knee

How is Lymphoma Diagnosed?
The diagnosis of lymphoma is usually confirmed by taking a sample from a lymph node, either by fine needle aspirate or biopsy. Fine needle aspirate of a superficial lymph node is a quick, simple procedure using a needle (similar to those used for booster injections) to collect cells from the node. It causes minimal discomfort and is normally carried out while a patient is awake or under mild sedation. In some cases a biopsy will need to be taken, involving the removal of a larger sample of tissue, this may be carried out under a general anaesthetic. These tests allow a very accurate assessment of the tumour by a specialist looking at the samples under a microscope.
To allow evaluation of internal lymph nodes and organs, patients usually have X-rays and an ultrasound scan. Mild sedation is usually required for these procedures, as patients need to be very still. Blood sampling is also performed to assess a patient’s general health status.
In some cases we will recommend taking samples of bone marrow to investigate whether or not cancer cells are present in the bone marrow. This procedure is carried out under a short general anaesthetic. All the diagnostic information obtained allows us to give an accurate prognosis and to discuss appropriate treatment options.
What Precautions Should I Take if my Pet has had Chemotherapy?
Chemotherapy agents can be excreted in the urine and faeces, and care must be taken when handling your pet’s waste. You will be advised of appropriate precautions to take at home, and it is important to note explicitly that pregnant women should avoid contact with the pet’s waste following chemotherapy.
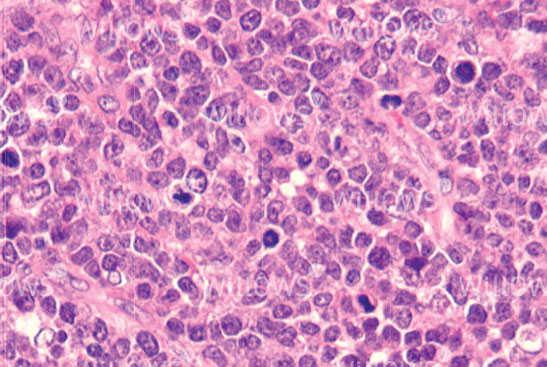
Fig 2: A fine needle aspirate sample of lymphoma cells seen under the microscope
What can I Expect if my Pet is treated for Lymphoma?
Unfortunately, chemotherapy for lymphoma is very unlikely to cure your pet, however it will allow a good quality of life to be enjoyed for some time.
Inevitably, the cancer cells become resistant to the drugs we use, and the cancer will come back. At this stage, it is often possible to get the cancer back under control for a while with alternative agents (this is known as a ‘rescue’ treatment). Eventually, the tumour cells will become resistant again and it is likely that your pet will have to be put to sleep when his or her quality of life deteriorates.
Hopefully, this will be after many happy months of good quality life for your pet and you to enjoy together.
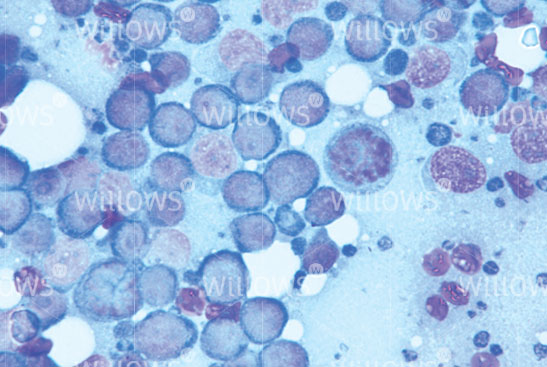
Fig 3: A solid biopsy of an affected lymph node, viewed under the microscope
What Treatments are Available for Lymphoma?
Lymphoma can be treated, however it is very uncommon for lymphoma to be cured, although treatment can make dogs feel well again for a period of time, with minimal side effects. This is called disease remission, when the lymphoma is not completely eliminated but is not present at detectable levels.
Without treatment, survival times for dogs with lymphoma are variable, depending on the tumour type and extent of the disease, but for the most common type of lymphoma the average survival time without treatment is four to six weeks. With current chemotherapy regimens such as the so-called Madison Wisconsin protocol, the average survival time is approximately 12 months.
Treatment options will be discussed in detail on an individual patient basis. The treatments available include:
Steroid treatment (Prednisolone): by itself this increases average survival times to one to three months, however it does not work in all cases. It will also make subsequent treatment with chemotherapy less successful.
Chemotherapy: using medications to stop or hinder cancer cells in the process of growth and division.
On each treatment day, before receiving chemotherapy, your pet’s progress is discussed, together with a full physical examination and blood tests. Following this assessment, chemotherapy doses are calculated and the drugs are administered either subcutaneously (under the skin), intravenously (into a vein) via a catheter, or orally.
Chemotherapy with the Madison Wisconsin protocol involves your pet having chemotherapy treatments weekly for nine weeks (with a one week break), then fortnightly up until six months (i.e. 25 weeks in total). At six months, if your dog is in remission, therapy will be discontinued. Chemotherapy can be restarted when a patient relapses i.e. when lymphoma comes back. Patients are individuals, so the response varies from case to case, as such, all patients receiving chemotherapy are carefully monitored and protocols adjusted to suit the individual.
What are the Potential Side Effects of Chemotherapy?
Side effects can be seen because chemotherapy agents damage both cancer and normal rapidly dividing cells. Normal tissues that are typically affected include the cells of the intestine, bone marrow (which makes the red blood cells, white blood cells and cell fragments involved in blood clotting called platelets) and hair follicles.
Hair loss is uncommon in dogs having chemotherapy, however it can be seen in certain breeds that have a continuously growing coat, such as Poodles and Old English Sheepdogs (cats rarely develop hair loss, but may lose their whiskers). Hair usually grows back once chemotherapy is discontinued. Damage to the cells of the intestines can result in changes in appetite or stool consistency and occasionally vomiting. Damage to the bone marrow reduces blood cell production, particularly infection fighting white blood cells (neutrophils).
Steroids are often used in combination with chemotherapy. These medications can make patients feel that they want to eat and drink more (especially during the first week of therapy when doses are usually higher and given every day). Patients should not have their access to drinking water restricted, however it is important not to increase their food intake, as excess weight gain can be problematic. The increased thirst is associated with increased urination, so patients may also need to go out to pass urine more often.
Cyclophosphamide, one of the commonly used chemotherapy agents, can cause irritation to the lining of the bladder, producing cystitis-like signs, so it’s important to bring urine samples when requested and to monitor your pet’s urination very carefully, and to promptly report any signs of problems.
Epirubicin, another chemotherapy agent, can cause damage to the heart muscle over time. The more doses your dog has, the greater the risk. For this reason, we will carry out checks on the heart before the drug is given for the first time and at various points during the treatment course. Heart complications are extremely uncommon and your dog is at much greater risk if the lymphoma is not treated.
Medications will be prescribed to help to prevent complications, and you will be advised on which signs to monitor. Compared to human patients who receive chemotherapy, pets experience fewer and less severe side effects, which can usually be managed at home. This is because a lower drug dose is given and not combined with as many drugs as in human medicine. Your pet’s quality of life is really important to us and to you.
What Signs Should I look out for if my Pet has had Chemotherapy?
Signs of gastrointestinal upset: if your pet has vomiting or diarrhoea for more than 24 hours please contact us or your local Vet. It is also important to watch for any dark coloured faeces.
Signs of bone marrow suppression: Neutrophils (infection fighting white blood cells) are at their lowest point usually five to seven days after treatment. If your pet is depressed, off its food, panting excessively or is hot to the touch at this time, please contact us.
Signs of bladder problems: you should alert us if your dog is urinating more frequently than previously, is straining or having difficulty passing urine, or if you see blood in the urine.
To save this page as a PDF, click the button and make sure “Save as PDF” is selected.
Cancer Care
Find out more
To assist owners in understanding more about Cancer Care we have put together a range of information sheets to talk you through the some of the more common conditions seen and treated by our Specialists.

